In the MIT lab of neuropharmacologist Richard Wurtman, rodents that received a new Alzheimer’s drug have shown a marked improvement in learning and memory. They are able to master elaborate mazes in half the time of their all-natural counterparts. Wurtman theorizes that the memory loss and dementia associated with Alzheimer’s disease is caused not by amyloid plaques and tangles but by a gradual deterioration of the brain’s synapses. Wurtman’s drug-a cocktail of three dietary supplements including uridine, choline, and an omega-3 fatty acid called DHA-is designed to generate more synapses. The three ingredients deliver the stimulus and raw material needed to create more phosphatidylcholine, a major component of neuronal membrane. More membrane, the thinking goes, means more neuronal encounters, more synapses, and more relayed messages. Wurtman’s cocktail has just entered a massive clinical trial involving 10,000 Alzheimer’s patients spread across 10 European countries. The same drug that could preserve brain function in Alzheimer’s patients also has potential as a memory drug for healthy people. This thesis explores the ethical questions surrounding such biotechnological enhancement. What might be the benefits and drawbacks of taking a memory booster? Could a class-like division eventually arise between those who get the drug and those who do not? Could the molecular manipulations of a smart drug-what some call “cosmetic pharmacology”–change qualities that are inextricable from who we are?
A Bright Idea?: The Promise and Peril of a Memory Drug

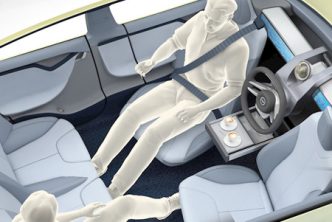
Could a class-like division eventually arise between those who get a memory drug and those who do not?