“When Going to the Bathroom Becomes Scary” received honorable mention for the DeWitt Wallace Prize for Science Writing for the Public.
What is diabetes?
One one-thousand. Two one-thousand. Three one-thousand. Four one-thousand.
Five one-thousand. Six one-thousand. Diabetes just claimed another life.
The International Diabetes Federation (IDF) reports that every six seconds–every six fleeting seconds–diabetes takes another person’s life. IDF further reports that, as of 2015, approximately 415 million adults have diabetes worldwide with close to half of such cases going undiagnosed; the number is projected to rise to 642 million by 2040.1 While the popular scapegoat for diabetes’s rise is the global obesity epidemic, the story is actually much more complicated. For one, “diabetes” is an umbrella term for two main forms of the disease: type 1 and type 2 diabetes. Even then, a myriad of factors can lead to a diabetic death sentence. Just as many variables and series of unfortunate events can lead to a particular type of cancer, so can many different factors lead to diabetes. Usually, our bodies do an amazingly complex job at managing how it absorbs the nutrients from the foods we eat. A few errors, here and there, can disrupt this streamlined process.
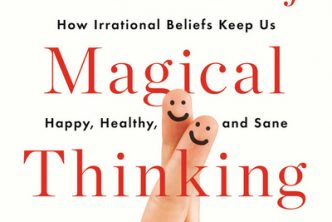
When a normal, healthy person eats a slice of sizzlingly savory Sicilian pizza, their stomach grinds and churns the pizza until the cheesy garlic crust and salty tomato sauce become one uneven ball of foodstuffs. That ball—more formally known as the “bolus”—then travels through the digestive system to be broken down even further. Starches eventually become glucose molecules; proteins become amino acids; fats become monoglycerides. In short, the digestive system breaks down food until the rest of our bodies can use it. Digestion, though seemingly inefficient, is necessary. Our bodies are made of roughly 37.2 trillion cells!2 Given the average size of a human cell,3 if we were to stretch out one person’s 37.2 trillion cells in a single-file line, that line would circle around Earth’s equator almost 19 times. And, well, we have to feed these hungry cells. Because the cells are so tiny, our digestive system must indeed break down the food we eat.
To feed baby Steve, would Mom give baby Steve a whole Granny Smith apple or mini-spoonfuls of applesauce? For now, let’s imagine Sicilian pizzas are apples (we can dream). The glucose molecules, amino acids, and monoglycerides are the “applesauce” that is digested pizza. After thoroughly digesting food, our bodies shuttle the nanoscopic nutrients to the rest of our body—our arteries and veins their highways. But how do our cells know when to “open their mouths” to take in the applesauce? Just as Mom says, “The Choo-Choo train is coming!” when spoon-feeding baby Steve applesauce, so does insulin—a protein-like hormone signal—tell our cells to take in nutrients from our bloodstream. This signaling either is missing or goes haywire when a person develops diabetes, which means that the cells can no longer take in nutrients normally and thus leave nutrients unused in the bloodstream. Most prominently, glucose, a simple sugar and our bodies’ favorite source of energy, aimlessly floats around in the bloodstream. Diabetes is a group of metabolic diseases wherein the body has consistently high blood glucose levels—lots of aimlessly floating blood sugar.
Anatomy of a metabolic syndrome and how to deal with it
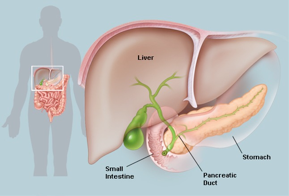
The pancreas is an awesome organ that sits right behind the stomach; it functions in both the digestive and endocrine system. Not only does the pancreas help absorb nutrients, but it also sends signals to the rest of the body to absorb those nutrients. The latter is controlled in a dual action manner by two signaling molecules, also known as hormones.
Endocrine, or signaling, functions of the pancreas are carried out by two hormones: insulin and glucagon. Two types of cells regulate the endocrine functions of the pancreas. In alpha cells, glucagon is made and secreted into the bloodstream; in beta cells, insulin is made and secreted into the bloodstream. When blood sugar levels are low—when wearily getting up from bed at 8:00 A.M. with a huge craving for sugary orange juice is real—glucagon regulates blood sugar levels by initializing a metabolic process called gluconeogenesis. Gluconeogenesis “newly generates” glucose, thereby increasing blood sugar levels. On the other hand, when blood sugar levels are high, insulin regulates blood sugar levels by signaling our bodies’ cells to take in sugar from our bloodstream. Hence, the two hormones are called antagonists to each other. Glucagon increases blood sugar levels, and insulin decreases blood sugar levels. Thus, too much glucagon or too little insulin signaling can cause high blood sugar—can cause diabetes. Usually, the latter is impaired in diabetics.
The pathology of type 1 and type 2 diabetes are markedly different. Type 1 diabetes often involves a problem with the immune system, which is the defense system built into our bodies that kills germs, removes cancer cells, and destroys whatnot, day-to-day. In nearly all of type 1 diabetes cases, the body is hyper-alert to foreign invaders.

This results in an unwanted immune response; hence, type 1 diabetes is categorized as an “autoimmune disorder.” The body quite literally attacks its own pancreas, mistaking the organ for a big “germ” and destroying it. In fact, type 1 diabetics are readily tested for other hormone levels, such as thyroid hormone, due to the relatively high likelihood that their immune systems are marking other endocrine organs for destruction, too. While the immune system ends up destroying beta cells, alpha cells are mysteriously “spared” from autoimmune attack, so glucagon manufacturing is still present.4 Therefore, type 1 diabetics are absolutely dependent on insulin for every day for the rest of their lives. Commonly, all of this happens when type 1 diabetics are in their younger years, so “rest of their lives” is all the more unfortunate. Accordingly, type 1 diabetes is also known as “juvenile diabetes.” Without insulin, type 1 diabetics cannot absorb nutrients and will eventually die if untreated; they carry the burden of insulin dependency for the rest of their lives.
Controlling blood sugar levels for type 1 diabetics is not an easy take-a-pill-a-day routine. Type 1 diabetics either have to inject insulin with needles, or “insulin pens,” several times every day or use insulin pumps.5 Unfortunately, “oral insulin” is only in its early stages of development; diabetes will have to stick with needles for a while yet.6 Needles aren’t even the annoying or scary part, though. It turns out that too much insulin can kill—yes, kill—anyone: having too-low blood sugar levels is dangerous, potentially resulting in diabetic comas and eventually death.
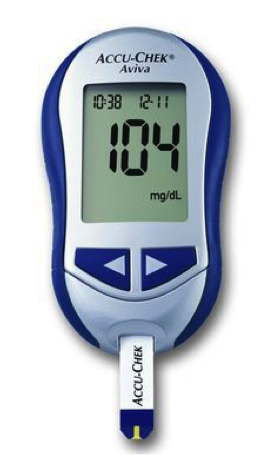
What’s worse, diabetics who have too-low blood sugar levels merely feel fatigued in the same way that people having heart attacks merely feel a slight tightening in their chests. And what’s even worse, simply not eating or exercising too much, by themselves, can cause low blood sugar. Indeed, type 1 diabetics tread on a frighteningly thin line of life and death: to avoid the side effects of high blood sugar levels— hyperglycemia—or to possibly die from low blood sugar levels—hypoglycemia—that is the shocking question. Recent advances in the biotechnology industry have, at least, made diabetics’ lives easier though. For example, continuous glucose monitors (CGMs) allow diabetics to monitor their blood sugar levels throughout the day, and these CGMs will hiss like threatened cats if diabetics were to dip to near-hypoglycemia levels of blood sugar.7 On the other hand, different types of clinically-available insulin variants have allowed diabetics to tune their blood sugar levels with more ease, such as slow-acting and rapid-acting insulins. A typical insulin regimen will consist of multiple insulins—say, one dose of slow-acting insulin per day and varying doses and number of doses of rapid-acting insulin depending on the amount of ingested carbohydrate per meal. Further up the drug-development pipeline, glucose-responsive insulin and glucose-responsive insulin delivery systems—novel self-regulating diabetes therapies currently being worked on at research powerhouses such as the Massachusetts Institute of Technology—are on their way.8
On the flip side, in type 2 diabetes, insulin is still present. The distinguishing factor between type 1 and type 2 diabetes is a simple question of, “Can the diabetic produce at least some insulin by him/herself?” However, type 2 diabetes has many flavors; type 2 diabetes can be thought of as a “not type 1 diabetes but still high blood sugar levels” category. In fact, at times, type 2 diabetes may not even involve insulin-signaling problems at all. Hyperglucagonemia, a state of excess glucagon secretion, can result in high blood sugar levels and not have to do with defects in insulin signaling.9
To enumerate all the “types” of type 2 diabetes would be overwhelming. Instead, acknowledging the main cause of type 2 diabetes is, in itself, very informative: insulin resistance, the quintessential cause for type 2 diabetes.
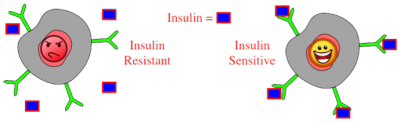
Insulin “sensitivity” is a relatively abstract measure of how readily our bodies’ cells recognize insulin. When insulin is made in the beta cells of the pancreas, secreted, and then shuttled to the rest of our bodies, our cells can be either eager or lazy to see insulin. Many of our cells have insulin receptors on them, and when the insulin receptors are in a state of, “Hey, insulin! Take in blood sugar now!” everything is fine. On the other hand, when these insulin receptors go, “Meh, insulin. Whatever,” type 2 diabetes occurs.
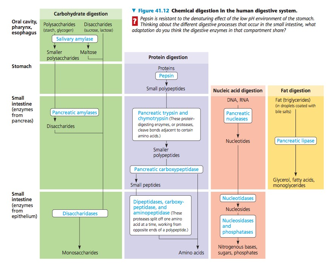
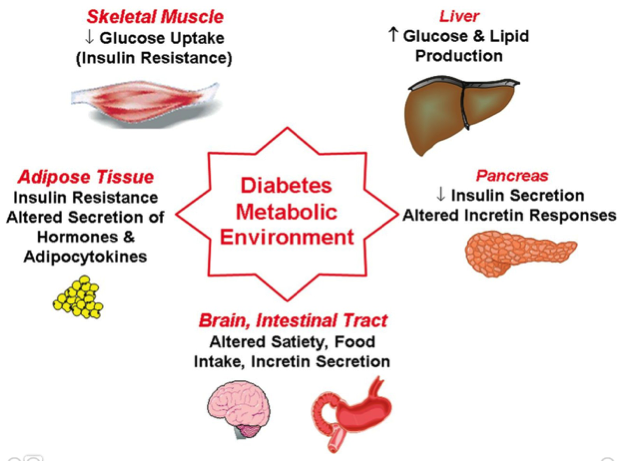
Hence, no matter how much insulin is being produced and secreted in type 2 diabetics’ pancreases, their bodies’ cells are too “resistant” to insulin in order to start taking in blood sugar. The mechanistic basis behind insulin resistance is a field of research under heavy investigation. For sure, one thing is clear though: insulin resistance can be caused by a multitude of factors. Most well known causes for insulin resistance include poor diet, lack of exercise, or other unhealthy lifestyle habits.
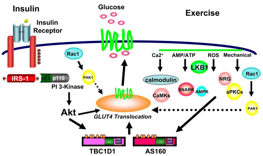
Resistance to insulin, in particular, lead to the well-known cardiovascular, or “heart,” diseases associated with diabetes. People who have type 2 diabetes are two to four times more likely to develop cardiovascular diseases.10 Type 2 diabetics’ likelihood for heart disease is, in part, attributable to the association of obesity and diabetes: poor diet, lack of exercise, and so forth cause diabetes and heart disease. Research on the biochemical explanation for insulin resistance causing heart disease has yielded fascinating implications. For one, recent research has shown that insulin’s actions within the vascular system carries an anti-atherogenic response.11 That is, insulin’s actions on cells prevent atherosclerosis, or fatty plaque deposition in the inner walls of arteries that ultimately “clog up” said arteries. Yes, insulin, mops up the plaque-y mess in arteries!
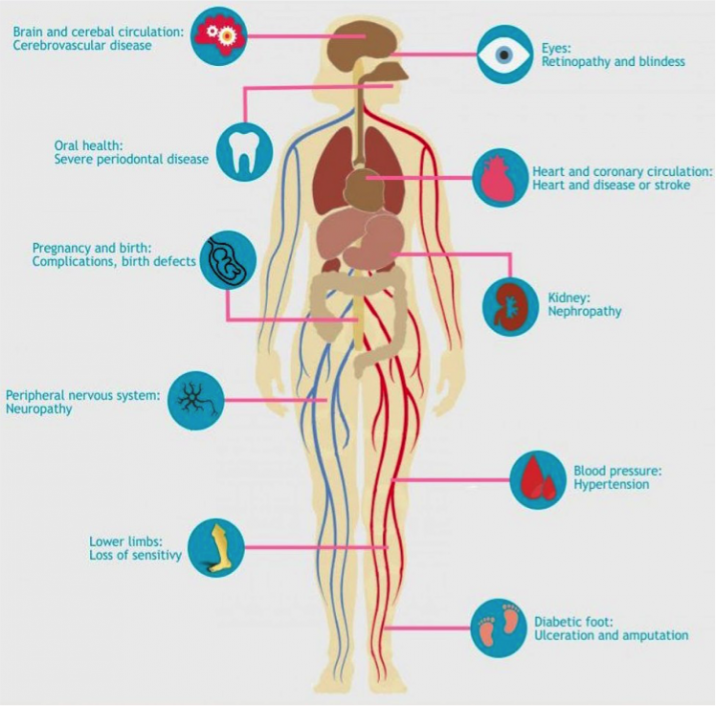
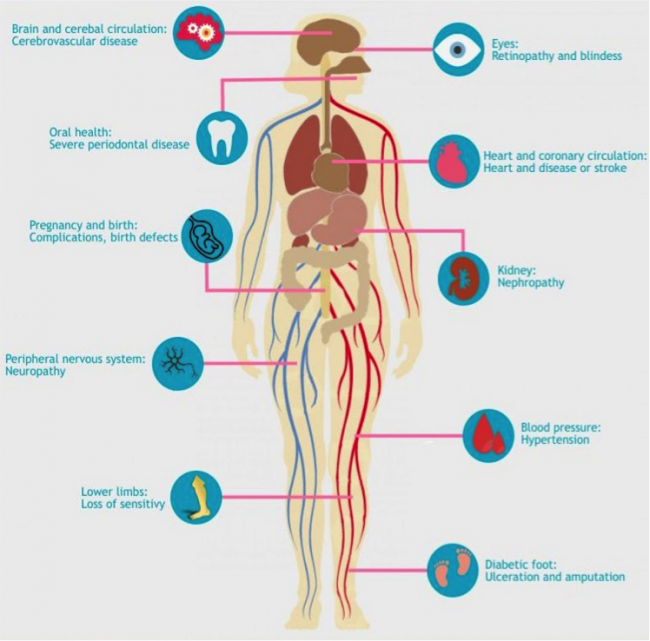
As scary as heart disease in type 2 diabetes may sound, diabetes has many other deleterious effects on the body—in both type 1 and type 2 diabetes. High blood pressure, nerve damage, blindness, strokes, and so on are all other common repercussions of uncontrolled blood sugar levels. In fact, diabetic blindness even has its own name: “diabetic retinopathy,” which happens when blood vessels within the eye start swelling up and bursting due to high blood sugar. But diabetes’s bad reputation for being an “obese disease” is a really unfair oversimplification.
Born this way
“Diabetic” and “obese” are definitely not synonymous. First and foremost, type 1 diabetes can, seemingly at random, affect nearly everyone; it’s an indiscriminate autoimmune disorder. A lot of type 1 diabetics are discreet about their diabetes in fear of being misunderstood—in fear of being labeled as “unhealthy” and “insensible” individuals. Moreover, while type 2 diabetes correlates strongly with obesity, for some type 2 diabetics, diabetes comes as a genuine surprise.
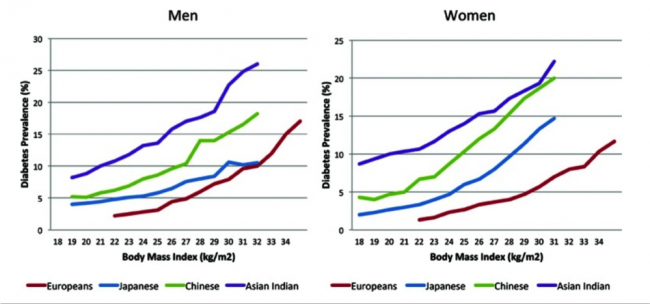
Certain individuals are at an alarmingly high risk for type 2 diabetes simply due to their lineage. In fact, ethnic-specific at-risk-for diabetes body mass index (BMI) cutoffs have been prescribed due to this fact.12 Whereas a BMI of greater than 30 kg/m2— “obese” in BMI standards—prompts attention for diabetes risk in White individuals, a BMI of 24 kg/m2 puts South Asians at-risk for diabetes. The figure is 25 kg/m2 and 26 kg/m2 for Chinese and Black individuals, respectively. In these relatively “skinny” type 2 diabetics, the problem can be attributed to the inherent distribution of body fat.13 Not all fat is physiologically as damaging: visceral fat, which surrounds our organs, is much more dangerous than subcutaneous fat, which lies directly under our skin. That is, visceral fat contributes more to the development of diabetes than does subcutaneous fat.
Birth also causes diabetes—no, not through being born with a predisposition for diabetes but the process of birth itself causes diabetes. It’s called gestational diabetes.14
One of the many risks that come with giving birth is developing diabetes. With care, gestational diabetes will not develop to type 2 diabetes, fortunately.15
Diabetes makes a great case study for “Nature vs. Nurture.”
To what extent do the A’s, T’s, G’s, and C’s in our genes influence our risk for diabetes? How much can the environment influence it? To what extent can food security reduce the likelihood of diabetes?16 The answers, of course, are not simple. But if possible, why not live a sensible, healthy life?
A cure? Cures?
It’s old; in fact, diabetes is one of the oldest-known diseases. Ancient Egyptian medical papyrus annals dating back to 1,500 B.C. chronicle diabetes. The ancient physicians noted that “sugary urine” would come from their diabetic patients; today, we know the “sugary urine” to be a direct cause of high blood sugar levels. By 1675, diabetes’s formal name, “diabetes mellitus,” was established—“diabetes” and “mellitus” meaning, “siphon [urine]” and “honey,” respectively.17 See? The name makes sense.
Before the discovery that insulin could be used to lower blood sugar levels, the best “treatment” would be to starve oneself, buying perhaps a year or two—at most. Dr. Frederick Banting and his student, Dr. Charles Best, changed diabetes forever in 1921 with their discovery that dog pancreas extract can lower blood sugar levels. The dog pancreas “extract” was the one-and-only insulin, and in 1923, Banting and a collaborator, Professor J.J.R. Macleod, were awarded Nobel Prizes in Physiology or Medicine for their discovery of insulin. Research in the field of diabetes has since grown dramatically.
From Dr. Rachmiel Levine’s discovery that insulin functions like a “key” to the insulin receptor to Nobel Prize winner Dorothy Hodgkin discovery of insulin’s molecular structure, diabetes has only become more bearable. As for a cure to diabetes, that may come soon, too.
Currently, the risks associated with pancreas transplants heavily outweigh the potential benefits that they can afford.18 Instead, a promising approach to curing diabetes is through the use of stem cells. One of the most prominent—if not, the most prominent—scientist tackling this approach to diabetes therapies is Professor Doug Melton, co-director of the Harvard Stem Cell Institute, founding co-chair of Harvard’s Department of Stem Cell and Regenerative Biology, and Xander Harvard University Professor. Ultimately, the dream that Melton and his scientific collaborators share is to use stem cells to create functioning beta cells that secrete insulin, effectively replacing the pancreas.
The project to create replacement beta cells involves Professor Dan Anderson, Samuel A. Goldblith Professor of Applied Biology and Professor of Chemical Engineering and Institutes for Medical Engineering and Science at the Massachusetts Institute of Technology.19 Research centers devoted to diabetes research, such as the Joslin Diabetes Center, only bring more optimism to the picture. One day: no more insulin injections, no more finger-pricking, no more nephropathy, no more hypoglycemic episodes, no more diabetes. One day.
Despite all odds, now, the question is not if diabetes can be cured. It’s when diabetes will be cured.
Disclaimer: The author of this writing is currently an undergraduate researcher in the Anderson Lab of the David H. Koch Institute for Integrative Cancer Research at the Massachusetts Institute of Technology. His family is afflicted by diabetes—most notably, his father who has type 2 diabetes and is insulin-dependent.
References
- IDF diabetes atlas – 7th edition. (n.d.). Retrieved April 03, 2017, from http://www.diabetesatlas.org/
- Bianconi E, Piovesan A, Facchin F, et al. An estimation of the number of cells in the human body. Ann Hum Biol. 2013;40(6):463-71.
- Reference Links for Key Numbers in Biology. (n.d.). Retrieved April 03, 2017, from http://bionumbers.hms.harvard.edu/KeyNumbers.aspx
- Anquetil F, Sabouri S, Thivolet C, et al. Alpha cells, the main source of IL-1β in human pancreas. J Autoimmun. 2017;14(2):45.
- Type 1 diabetes Treatments and drugs. (n.d.). Retrieved April 03, 2017, from http://www.mayoclinic.org/diseases-conditions/type-1-diabetes/basics/treatment/con-20019573
- Medically Reviewed by Zara Risoldi Cochrane, PharmD, MS, FASCP on December 21, 2016 — Written by Kimberly Wonderly. (2016, December 21). Could Oral Insulin Be an Option Some Day? Retrieved April 02, 2017, from http://www.healthline.com/health/type-2-diabetes/oral-insulin
- Continuous Glucose Monitoring | NIDDK. (n.d.). Retrieved April 03, 2017, from https://www-niddk-nih-gov.ezproxy.canberra.edu.au/health-information/diabetes/overview/managing-diabetes/continuous-glucose-monitoring
- Getting to Glucose Responsive Insulin – How. (2016, May 31). Retrieved April 03, 2017, from https://diatribe.org/getting-glucose-responsive-insulin-%E2%80%93-how-%E2%80%9Csmart%E2%80%9D-will-it-be
- Godoy-matos AF. The role of glucagon on type 2 diabetes at a glance. Diabetol Metab Syndr. 2014;6(1):91.
- Diabetes. (n.d.). Retrieved April 03, 2017, from http://www.world-heart-federation.org/cardiovascular-health/cardiovascular-disease-risk-factors/diabetes/
- King GL, Park K, Li Q. Selective Insulin Resistance and the Development of Cardiovascular Diseases in Diabetes: The 2015 Edwin Bierman Award Lecture. Diabetes. 2016;65(6):1462-71.
- Chiu, M., Austin, P. C., Manuel, D. G., Shah, B. R., & Tu, J. V. (2011). Deriving Ethnic-Specific BMI Cutoff Points for Assessing Diabetes Risk. Diabetes Care, 34(8), 1741–1748. http://doi.org.ezproxy.canberra.edu.au/10.2337/dc10-2300
- Araneta, M. R. G. and Barrett-Connor, E. (2005), Ethnic Differences in Visceral Adipose Tissue and Type 2 Diabetes: Filipino, African-American, and White Women.
- Obesity Research, 13: 1458–1465. doi:10.1038/oby.2005.176
- Gestational Diabetes. (n.d.). Retrieved April 03, 2017, from http://www.niddk.nih.gov.ezproxy.canberra.edu.au/health-information/health-communication-programs/ndep/am-i-at-risk/gdm/gestational-diabetes-pregnancy/Pages/publicationdetail.aspx
- Gestational Diabetes After Birth. (n.d.). Retrieved April 03, 2017, from http://www.webmd.com/diabetes/gestational-diabetes-guide/gestational-diabetes-after-birth
- Gucciardi, E., Vahabi, M., Norris, N., Del Monte, J. P., & Farnum, C. (2014). The Intersection between Food Insecurity and Diabetes: A Review. Current Nutrition Reports, 3(4), 324–332. http://doi.org.ezproxy.canberra.edu.au/10.1007/s13668-014-0104-4
- Poretsky, L. (2016). Principles of diabetes mellitus (2nd ed.). Place of publication not identified: Springer.
- Anne Trafton | MIT News Office. (2016, January 25). No more insulin injections? Retrieved April 03, 2017, from http://news.mit.edu.ezproxy.canberra.edu.au/2016/pancreatic-cells-diabetes-treatment-insulin-injections-0125
- Stanford KI, Goodyear LJ. Exercise and type 2 diabetes: molecular mechanisms regulating glucose uptake in skeletal muscle. Adv Physiol Educ. 2014;38(4):308-14. Stanford KI, Goodyear LJ. Exercise and type 2 diabetes: molecular mechanisms regulating glucose uptake in skeletal muscle. Adv Physiol Educ. 2014;38(4):308-14. Pancreas transplant. (n.d.). Retrieved April 03, 2017, from https://medlineplus.gov/ency/article/003007.htm
Figures
[Fig. 1] Reece, J. B., & Campbell, N. A. (2014). Campbell biology (8th ed.). Boston: Benjamin Cummings.
[Fig. 2] Stanford KI, Goodyear LJ. Exercise and type 2 diabetes: molecular mechanisms regulating glucose uptake in skeletal muscle. Adv Physiol Educ. 2014;38(4):308-14.
[Fig. 3] Hoffman, M. (n.d.). Pancreas. Retrieved April 03, 2017, from http://www.webmd.com/digestive-disorders/picture-of-the-pancreas
[Fig. 4] 5 Types of Insulin and How They Work. (n.d.). Retrieved April 03, 2017, from http://www.health.com/health/gallery/0,,20402402,00.html
[Fig. 5] Accu-Chek Glucose Monitor Clip Art
[Fig. 6] Berlanga-Acosta J, López-Saura P, Guillen-Pérez I, Guillen-Nieto G, Acevedo-Castro B, et al. (2013) Type 2 Diabetes Mellitus (T2DM): Biological Overview from Pathways to Organelles and its Translation toward a Torpid Wound Healing Process. J Diabetes Metab 4:285. doi: 10.4172/2155-6156.1000285
[Fig. 7] Spliced cell cartoons with Clip Art, ClipArtBest
[Fig. 8] Effects of Diabetes. (n.d.). Retrieved April 03, 2017, from http://visual.ly/effects-diabetes
[Fig. 9] Ma, R. C., & Chan, J. C. (2013). Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Annals of the New York Academy of Sciences, 1281(1), 64–91. http://doi.org.ezproxy.canberra.edu.au/10.1111/nyas.12098
[Fig. 10] Jin W, Patti ME. Genetic determinants and molecular pathways in the pathogenesis of Type 2 diabetes. Clin Sci. 2009;116(2):99-111.
[Fig. 11] Pagliuca, Felicia W. et al. Cell , Volume 159 , Issue 2 , 428 – 439